Where Reps Meet Referrals: How Fitness and Healthcare Are Finally Teaming Up

By Lydia Chan
The line between clinical care and wellness isn’t blurring — it’s being intentionally erased. In recent years, personal trainers, health coaches, nutritionists, and nurse practitioners have begun working in concert, not competition. Together, they’re building something closer to real support: not just treating problems, but helping people avoid them in the first place. This isn’t a theoretical shift. It's showing up in how gym memberships are prescribed, how care teams are assembled, and how chronic conditions are managed day to day. What we’re watching isn’t just the integration of industries. It’s the slow construction of a health system that starts earlier, stays longer, and sees the whole person.
Fitness Meets Medicine
Your local gym might be more clinical than you think — and that’s intentional. Across the country, we’re seeing the rise of physician‑guided fitness programs where workouts aren’t just about aesthetics but prescriptions. Trainers work alongside physical therapists, and plans are built around diagnoses, not just desires. This isn't about taking medicine with your deadlifts. It’s about reclaiming movement as a legitimate medical tool — one that can be measured, monitored, and managed. These programs are closing the gap between “go see your doctor” and “start exercising,” by turning both into the same appointment.
Health Coaches in Clinics
There was a time when “going to the doctor” meant 12 minutes with a rushed provider and a vague plan. That’s starting to crack. In integrated models, health coaches now relieve providers and share care — not by doing less, but by doing what clinicians can’t. Coaches take time. They ask different questions. They track behavior, motivation, context. The physician might explain what needs to change. The coach stays to explore how. In clinics from Seattle to St. Louis, coaches are no longer an optional luxury. They’re the continuity glue — stitching clinical insight to real-world change.
Nurse Practitioners and Wellness Alignment
Inside this shift, one role has become quietly central: the family nurse practitioner. With clinical authority and a community-first mindset, they’re trained to span the gap between primary care and lifestyle support. Those pursuing an online FNP degree are now preparing for a hybrid reality — one where wellness literacy, coaching coordination, and patient education are core to the job. It’s not about handing off patients to coaches and hoping for the best. It’s about co-designing plans that reflect both clinical insight and daily life. FNPs are emerging not just as care providers, but as system integrators — a crucial link in the whole-person chain.
Shared Wellness Workspaces
Forget the strip mall. The new wellness hub is a collective — yoga instructors, mental health therapists, RDNs, and bodyworkers — independent practitioners sharing space and, more importantly, sharing clients. It’s not a referral machine. It’s a support lattice. Someone walks in with back pain, walks out with a trainer, a therapist, and a plan that doesn’t bounce between buildings or inboxes. This physical proximity invites collaboration, but also curiosity. When disciplines coexist, they tend to coevolve. The result is not a jack-of-all-trades — it’s a circle of specialists who understand each other's rhythms.
From Advice to Action
Medical advice without action is just paperwork. Health coaches are increasingly stepping in to help implement physician‑recommended changes — translating prescriptions into food choices, fitness habits, and daily decisions. It’s not about nagging. It’s about witnessing. The accountability comes from presence, not pressure. Coaches aren’t there to repeat the doctor’s words — they’re there to hear the client’s, and help build a bridge between the two. In practice, this means fewer patients saying, “I don’t know what to do,” and more saying, “Here’s what I did last week.”
Beyond One Specialty
Whole-person health isn’t a buzzword when it’s operationalized. Forward-leaning clinics now combine mental, behavioral, and primary care into a single fabric — one where patients don’t get bounced around or siloed out of their own story. Instead, care plans are shared. Notes are integrated. Teams aren’t just co-located — they’re co-invested. The result isn’t perfect harmony. It’s intentional friction — the kind that surfaces blind spots and forces practitioners to adjust. And for patients, it finally feels like someone’s seeing the connections they’ve known were there all along.
Healthcare‑Wellness Brand Teams
This collaboration isn’t limited to small clinics or boutique wellness centers. At scale, we’re seeing health insurers and corporate wellness platforms merge missions. The Cigna and Virgin Pulse collaboration is one such example: insurers building prevention into the benefits stack, and wellness brands getting serious about outcomes. The goal? Replace the episodic nature of care with continuous engagement. Your workout streak might soon matter as much as your cholesterol reading — because both tell a story about long-term health resilience. It’s a shift from crisis response to capacity building, and the industry is finally investing in it.
We’re watching the rebuild of health, one unlikely alliance at a time. What used to be separate worlds — the gym, the doctor’s office, the therapist’s couch — are now interwoven. Not perfectly. Not uniformly. But undeniably. In these new networks, care is no longer something that happens to you, at a single point in time. It’s something you co-create, continuously, with a web of professionals whose shared language is outcomes. The best part? This isn’t just about adding services. It’s about removing gaps. And for the first time in a long time, that feels like care.
Discover the life-changing solutions at Dansons Medical, and empower your loved ones with the independence and comfort they deserve.
- Dansons Medical Support


 Lifts
Lifts
 Patient Lifts
Patient Lifts
 Stand Assists
Stand Assists
 Standing Aids
Standing Aids
 Slings
Slings
 Parts & Accessories
Parts & Accessories
 Wheelchairs
Wheelchairs
 Ergonomic
Ergonomic
 Portable
Portable
 Reclining
Reclining
 Standing
Standing
 Sporting
Sporting
 Bariatric
Bariatric
 Ramps
Ramps
 Modular
Modular
 Portable
Portable
 Parts & Accessories
Parts & Accessories
 Walking Aids
Walking Aids
 Rollator Walkers
Rollator Walkers
 Canes
Canes
 Crutches
Crutches
 Parts & Accessories
Parts & Accessories
 Scooters
Scooters
 4-Wheel
4-Wheel
 Folding
Folding
 Parts & Accessories
Parts & Accessories
 Nursing
Nursing
 Pregnancy Comfort
Pregnancy Comfort
 Self-Care
Self-Care
 Pump Parts
Pump Parts
 Exercise Equipment
Exercise Equipment
 Treadmills
Treadmills
 Walking Pads
Walking Pads
 Rowing Machines
Rowing Machines
 Strength & Conditioning
Strength & Conditioning
 Massage Chairs
Massage Chairs
 Saunas
Saunas
 Hot & Cold Tubs
Hot & Cold Tubs
 Stethoscopes
Stethoscopes
 Surgical Instruments
Surgical Instruments
 Forceps
Forceps
 Scalpels
Scalpels
 IV Poles
IV Poles
 Oxygen
Oxygen
 Beds
Beds
 Electric Beds
Electric Beds
 Standing Beds
Standing Beds
 Mattresses
Mattresses
 Bed Accessories
Bed Accessories
 Bed Parts
Bed Parts
 Chairs
Chairs
 Medical Recliners
Medical Recliners
 Phlebotomy Chairs
Phlebotomy Chairs
 Stools & Task Chairs
Stools & Task Chairs
 Parts & Accessories
Parts & Accessories
 Tables
Tables
 Overbed Tables
Overbed Tables
 Medical Tables
Medical Tables
 Recovery Couches
Recovery Couches
 Cabinets
Cabinets
 Pool
Pool
 Pool Lifts
Pool Lifts
 Pool Fitness & Therapy
Pool Fitness & Therapy
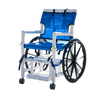 Pool Access Chairs
Pool Access Chairs
 Slings
Slings
 Parts & Accessories
Parts & Accessories
 Bath
Bath
 Toileting Aids
Toileting Aids
 Bath Lifts
Bath Lifts
 Shower Seats
Shower Seats
 Parts & Accessories
Parts & Accessories
 Portable Shower
Portable Shower
 Dansons Products
Dansons Products
 Transfer Aids
Transfer Aids
 Cushions
Cushions
 eBooks
eBooks
 Helpful Articles
Helpful Articles
 Reviews
Reviews
 Contact Us
Contact Us
 Create Account
Create Account
 Request a Quote
Request a Quote

Comments 0